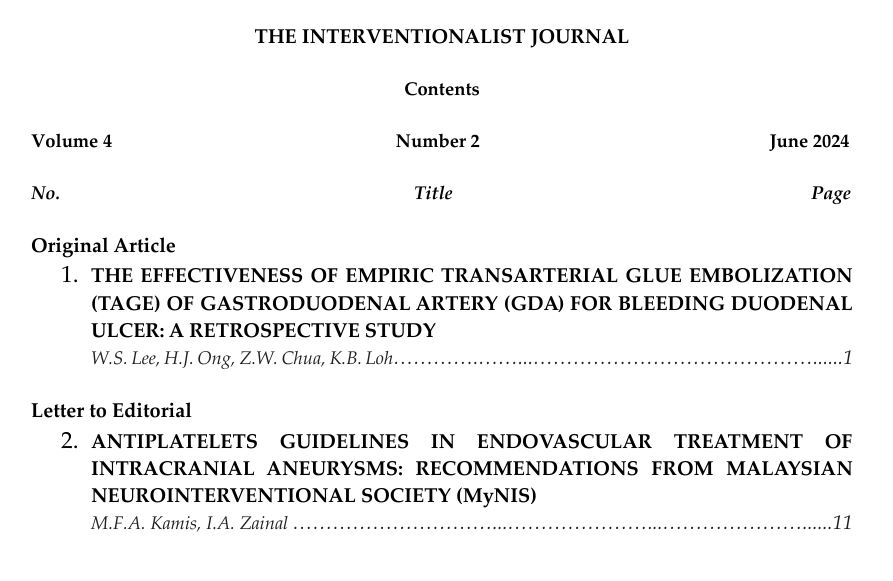
The Effectiveness of Empiric Transarterial Glue Embolization (TAGE) of Gastroduodenal Artery (GDA) for Bleeding Duodenal Ulcer
A Retrospective Study
DOI:
https://doi.org/10.32896/tij.v4n2.1-10Keywords:
empiric transarterial glue embolisation, gastroduodenal artery, bleeding duodenal ulcersAbstract
ABSTRACT:
Purpose
To conduct a clinical audit on clinical outcome of empiric transarterial glue embolization (TAGE) of gastroduodenal artery (GDA) for bleeding duodenal ulcers to evaluate treatment efficacy.
Materials and Methods
All patients treated for bleeding duodenal ulcers between June 2019 and June 2023, in a single tertiary center (Penang General Hospital) were identified based on intervention radiological reports. Patients with bleeding duodenal ulcers underwent empiric transarterial glue embolization (TAGE) of gastroduodenal artery (GDA) following endoscopic hemostasis were included. Information was extracted from patients' medical records, endoscopic and radiological reports. Data was computed and analyzed using Statistical Package for Social Sciences (SPSS).
Results
During the study period, a total of 26 patients were planned for empiric transarterial glue embolisation (TAGE) of gastroduodenal artery (GDA) for bleeding duodenal ulcer. The median age was 68 with 68% male (n=18) and 32% female (n=8). A total of 25 patients with duodenal ulcers of Forrest 1a (n=5), 1b (n=12), 2a (n=4), 2b (n=3) and 2c (n=1) who successfully underwent prophylactic TAGE of GDA were included in this study. It has a high technical success rate of 96.2% (n=25) with only one case of failure in cannulation due to tortuous arterial anatomy. Clinical success rate amongst the 25 patients who successfully underwent empiric TAGE of GDA was 84% (n=21) with only four patients developed rebleeding and required repeated endoscopic clipping. One of the four patients succumbed secondary to refractory bleeding.
Conclusion
Empiric transarterial glue embolisation (TAGE) of gastroduodenal artery (GDA) can be a useful adjunct treatment option in high risk bleeding duodenal ulcer with high technical and clinical success.
References
Palmer K, Atkinson S, Donnelly M, Forbes-Young R, Gomez C, Greer D, Halligan K, Hauser M, McPherson S, McCord M, et al. Acute upper gastrointestinal bleeding: management. UK: National Institute for Health and Clinical Excellence.
Hastings GS. Angiographic localization and transcatheter treatment of gastrointestinal bleeding. Radiographics 2000;20:1160–1168.
Management of non-variceal upper gastrointestinal bleeding. (2003). Ministry of Health Malaysia.
de Groot, N. L., van Oijen, M. G. H., Kessels, K., Hemmink, M., Weusten, B. L. A. M., Timmer, R., Hazen, W. L., van Lelyveld, N., Vermeijden, R. R., Curvers, W. L., Baak, B. C., Verburg, R., Bosman, J. H., de Wijkerslooth, L. R. H., de Rooij, J., Venneman, N. G., Pennings, M., van Hee, K., Scheffer, B. C. H., & van Eijk, R. L. (2014). Reassessment of the predictive value of the Forrest classification for peptic ulcer rebleeding and mortality: can classification be simplified? Endoscopy, 46(1), 46–52. https://doi.org/10.1055/s-0033-1344884
Boros, E., Sipos, Z., Hegyi, P., Teutsch, B., Levente Frim, Szilárd Váncsa, Kiss, S., Fanni Dembrovszky, Eduard Oštarijaš, & Shawyer, A. (2021). Prophylactic transcatheter arterial embolization reduces rebleeding in non-variceal upper gastrointestinal bleeding: A meta-analysis. World Journal of Gastroenterology, 27(40), 6985–6999. https://doi.org/10.3748/wjg.v27.i40.6985
Pyeong Hwa Kim, Jiaywei Tsauo, Ji Hoon Shin, & Yun, S.-C. (2017). Transcatheter Arterial Embolization of Gastrointestinal Bleeding with N-Butyl Cyanoacrylate: A Systematic Review and Meta-Analysis of Safety and Efficacy. Journal of Vascular and Interventional Radiology, 28(4), 522-531.e5. https://doi.org/10.1016/j.jvir.2016.12.1220
Loffroy R. Embolization for Upper GI Bleeding [Internet]. Endovascular Today; 2016. Available from: https://evtoday.com/articles/2016-apr/embolization-for-upper-gi-bleeding#:~:text=Glue%20embolization%20of%20the%20GDA
Hill, H., Beecham Chick, J. F., Hage, A., & Srinivasa, R. N. (2018). N-butyl cyanoacrylate embolotherapy: techniques, complications, and management. Diagnostic and Interventional Radiology. https://doi.org/10.5152/dir.2018.17432
Kuyumcu, G., Latich, I., Hardman, R., Fine, G., Oklu, R., & Quencer, K. (2018). Gastroduodenal Embolization: Indications, Technical Pearls, and Outcomes. Journal of Clinical Medicine, 7(5), 101. https://doi.org/10.3390/jcm7050101
Aina, R., Oliva, V. L., Therasse, E., Perreault, P., Bui, B. T., Dufresne, M.-P., & Gilles Soulez. (2001). Arterial Embolotherapy for Upper Gastrointestinal Hemorrhage: Outcome Assessment. Journal of Vascular and Interventional Radiology, 12(2), 195–200. https://doi.org/10.1016/s1051-0443(07)61825-9
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.